President Biden and Democratic Lawmakers Are Lowering Health Care Costs and Giving Families the Relief They Need
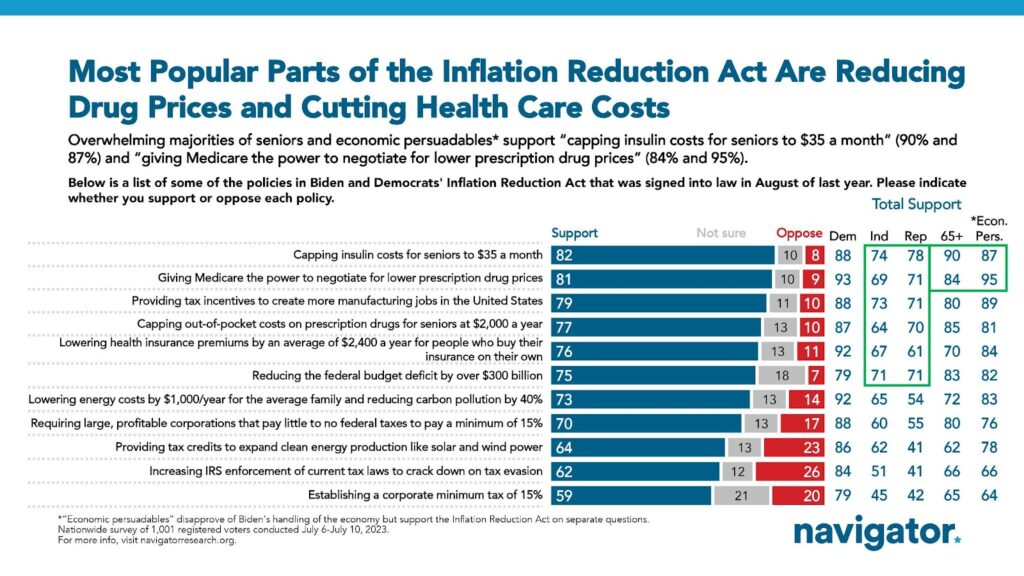
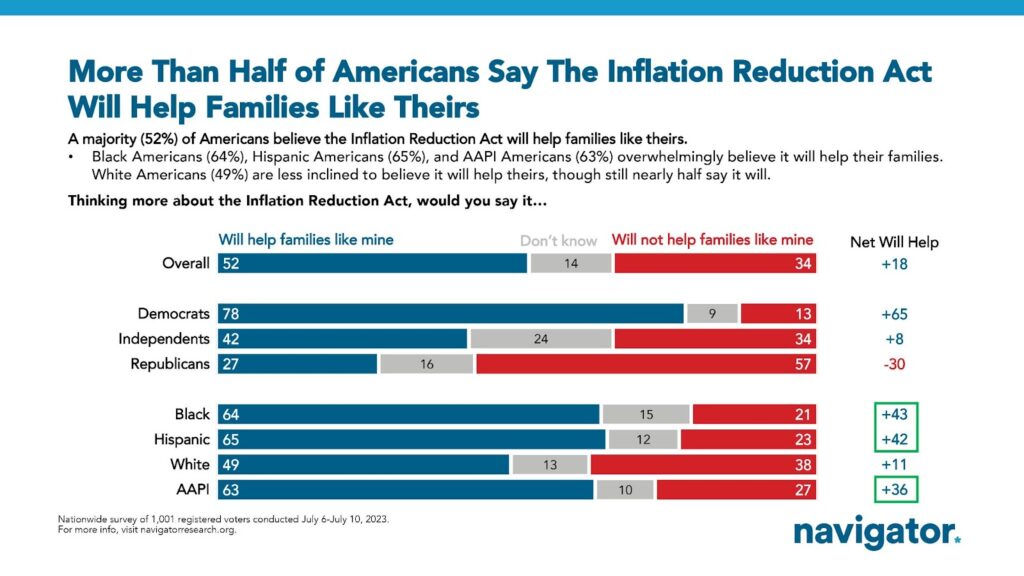
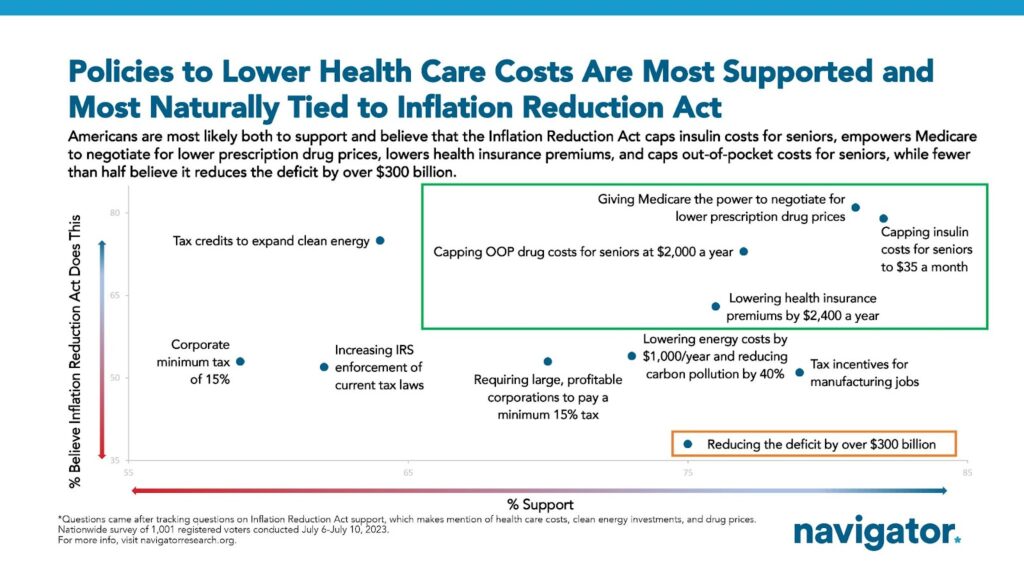
One year ago, President Biden signed the Inflation Reduction Act into law, driving down health care costs for seniors and families nationwide. This was a huge win in the ongoing fight for affordable health care. Between lowering premium costs for families by $2,400 on average, capping insulin costs, and stopping drug companies’ egregious price hikes, the new legislation is already working for the American people. Soon, seniors’ drug costs will be capped at $2,000 annually, and Medicare will finally be able to negotiate lower drug prices.
However, Republicans refuse to give up on their war on health care. They have reverted to some of the oldest tricks in the book and introduced numerous bills to repeal the Inflation Reduction Act and put drug and insurance companies back in charge. Meanwhile, in the courts, big drug companies have filed lawsuits against the federal government to try to stop Medicare from negotiating lower prices for millions of seniors.
Here’s what Democrats are saying about the anniversary of their historic victory:
BIDEN ADMINISTRATION
President Joe Biden: “One year ago, on August 16, 2022, President Biden signed the Inflation Reduction Act into law…The Inflation Reduction Act is a transformative law that is helping the United States meet its climate goals and strengthen energy security, investing in America to create good-paying jobs, reducing energy and health care costs for families, and making the tax code fairer. […] Nearly 15 million people are saving an average of $800 per year on their health insurance premiums, the nation’s uninsured rate has reached a historic low, and millions of seniors on Medicare are paying less in out-of-pocket costs for prescription drugs—including insulin, which is capped at $35 per month. […] The Inflation Reduction Act advances President Biden, Vice President Harris, and Congressional Democrats’ longstanding commitment to making health care more affordable for American families and seniors. The law is bringing down health care costs and thanks to President Biden, Vice President Harris, and the Inflation Reduction Act’s continuation of important improvements on the Affordable Care Act, the nation’s uninsured rate has reached an historic low, and nearly 15 million people are saving an average of $800 per year on their insurance premiums.” [White House Press Release, 8/16/23]
Department of Health and Human Services Secretary Xavier Becerra: “The first anniversary of the Inflation Reduction Act is cause for celebration, as millions of Americans are already saving money on health care. As a result of this law, individuals purchasing Marketplace coverage are paying less in premiums, people with Medicare are benefiting from the $35 cap on insulin, and saving on free, recommended vaccines, and we are strengthening Medicare for the next generation. The Biden-Harris Administration is delivering lower prescription drug costs, making health insurance more affordable, and making the economy work for working families.” [Department of Health and Human Services Press Release, 8/16/23]
The Centers for Medicare & Medicaid Services (CMS) Administrator Chiquita Brooks-LaSure: “The historic Inflation Reduction Act builds on the Biden-Harris Administration’s efforts to make health care more affordable and accessible that are life changing for millions of Americans. On this first anniversary of the Inflation Reduction Act, Americans are seeing the benefits – such as free recommended vaccines, lower insulin costs, and the enhanced tax credits that help more people afford their premiums in the Marketplaces.” [Department of Health and Human Services Press Release, 8/16/23]
U.S. CONGRESS
Senate Majority Leader Chuck Schumer (D-NY): “The Inflation Reduction Act was one of the most consequential pieces of legislation passed in decades, and in just one year it’s already paying huge dividends for the American people, for our economy, and for our climate. Democrats are proud of the progress we’ve made in implementing our agenda, and we will keep working until every American feels the benefits.” [Senate Democratic Caucus Press Release, 7/27/23]
House Democratic Whip Katherine Clark (D-MA-5): “One year ago, President Biden and Congressional Democrats enacted the Inflation Reduction Act to make good on our promise of progress and prosperity for everyday Americans — and we are proud to see that it is already delivering. In just its first year, the Inflation Reduction Act has slashed the cost of insulin to $35 per month for seniors and secured affordable health coverage for nearly 15 million Americans — saving them an average of $800 a year. It has spurred over $270 billion in private sector investments, creating more than 170,000 good-paying, green jobs in 44 states. And it has injected fairness into our tax system, ensuring billionaires and wealthy corporations pay their fair share — all while paving our path toward a carbon-free, climate-resilient future. Democrats know the best way to grow America’s economy is by growing the middle class. Through the Inflation Reduction Act, we are cutting costs and building the stronger, safer, more sustainable future that Americans deserve.” [House Democratic Whip Katherine Clark Press Release, 8/16/23]
Speaker Emerita Nancy Pelosi (D-CA-11): “When President Biden affixed his signature to the Inflation Reduction Act one year ago today, America not only made history – but we made progress on the most pressing challenge of our times. […] At the same time, families are feeling the impact of this landmark law at their kitchen table. At long last, Medicare will soon have the power to negotiate the price of prescription drugs. Seniors can now get insulin for just $35 a month. And fifteen million Americans are saving an average of $800 per year on health insurance through ACA exchanges.” [Speaker Emerita Nancy Pelosi Press Release, 8/16/23]
Senator Bob Casey (D-PA), Chair of the Special Committee on Aging: “One year ago, Democrats enacted the Inflation Reduction Act to fulfill President Biden’s promise to lower costs for families and tackle the climate crisis. Because of this law, seniors and families are spending less on their prescription drugs, Americans are spending less on their electricity bills, and we’re on the cusp of a manufacturing renaissance in the United States. By investing in America’s clean energy capabilities, we’re on track to meet our climate goals. Pennsylvania families and communities are feeling the impacts of the Inflation Reduction Act, but I’m proud to say that the best of this law is yet to come.” [Senator Bob Casey Press Release, 8/16/23]
Representative Frank Pallone (D-NJ-06), Ranking Member of the Committee on Energy & Commerce: “The Inflation Reduction Act is delivering for the American people, and it will continue to do so for years to come. The law is making prescription drugs and health care more affordable for millions of American families. Already this year, seniors are paying less for lifesaving insulin as the law caps the cost at $35 per month. Now, pharmaceutical companies have followed suit and are lowering the cost of insulin for more Americans, something that simply would not have happened without the passage of this law. Drug companies are also being forced to pay penalties when they raise prices above the rate of inflation, which has resulted in seniors receiving discounts on 43 drugs so far this year. And next month, the Department of Health and Human Services will announce the first 10 drugs it plans to negotiate lower prices on so seniors are no longer paying outrageously high prices. It is also dramatically lowering the cost of monthly health insurance premiums for millions of Americans, with four in five customers able to find health care coverage for $10 or less per month on HealthCare.gov.” [Representative Frank Pallone Press Release, 8/16/23]
Representative Richard Neal (D-MA-1), Ranking Member of the Committee on Ways and Means: “This first anniversary serves as a powerful reminder of what Democrats could achieve for the American people with a tight majority and goes to show, that where there’s a will there’s a way. From capping the cost of insulin for seniors to unlocking a new era of service at the IRS or spurring the single largest federal investment in climate action, the IRA is chock full of wins for the American people. Ways and Means Democrats proudly led on so much of this landmark law—saving families an average of $2400 on their health premiums, allowing Medicare to negotiate drug prices for the first time, and driving historic manufacturing and energy investments—and responsibly funded it by holding the wealthiest corporations accountable for their fair share. […] The promise of the Inflation Reduction Act shines bright after its first year and is only getting brighter.” [Representative Richard Neal Press Release, 8/16/23]
Senator Bob Menendez (D-NJ): “A year ago today, President Biden signed the Inflation Reduction Act into law. This historic legislation, which I was proud to support, was designed to lower costs, grow the middle class, and invest in our nation’s green energy future – and it is delivering on its promise. […] In the year since, seniors are paying less at the pharmacy counter, families are seeing reductions in their monthly energy bills, and the nation is pivoting faster than expected towards clean energy while we combat the global climate crisis. Simply put, our efforts are paying dividends for the American people, for the economy, and for the environment. The Inflation Reduction Act is a prime of example of what is possible when we prioritize helping hardworking families thrive.” [Senator Bob Menendez Press Release, 8/16/23]
Senator Joe Manchin (D-WV): “The Inflation Reduction Act (IRA) is one of the most historic pieces of legislation passed in decades for working and middle class families, and we are already seeing real results across West Virginia. While some across both parties and the Administration have chosen to play political games with this important legislation, the IRA included $238 billion in debt reduction, lowered the cost of prescription drug prices for millions of seniors – including more than 400,000 West Virginians on Medicare, capped insulin at $35 for seniors, and secured permanent funding for the Black Lung Disability Trust Fund.” [Senator Joe Manchin Press Release, 8/16/23]
Senator Tammy Baldwin (D-WI): “The Inflation Reduction Act is making a real difference in the lives of Wisconsin’s working families, and I am proud to have voted for it. Seniors across Wisconsin are saving hundreds of dollars a month on the cost of their prescription drugs because we took on big drug companies and capped the cost of insulin at $35 per month. Hundreds of thousands of Wisconsinites are saving on their monthly health care premiums. […] Big corporations are finally paying their fair share of taxes and we are cutting the deficit. I know we have more work to do to lower costs for families, but I am proud that our Inflation Reduction Act is delivering needed relief for working families and growing our Made in Wisconsin economy.” [Senator Tammy Baldwin Press Release, 8/16/23]
Senator Alex Padilla (D-CA): “[F]amilies are seeing the cost of life-saving medications lowered and the American Rescue Plan’s Affordable Care Act premium subsidies extended — preventing nearly one million low-income Californians’ premium costs from doubling. And we are funding these efforts by requiring billion-dollar corporations to finally pay their fair share in taxes. Thanks to the IRA, one year later we are celebrating reduced costs for working families and historic climate and health care investments in America. This is why the American people sent us to Congress — and why we will continue working to build on this historic progress — so that Californians have more money in their pockets, cleaner air to breathe, and a healthier future ahead.” [Senator Alex Padilla Press Release, 8/16/23]
Senator Peter Welch (D-VT): “The passage of the Inflation Reduction Act was a win for Vermont families, our economy, and the green energy future–and one year later it’s clear this law is delivering on its promises for our communities. We worked closely with the Biden Administration to include key Vermont priorities in this bill–including provisions to lower the cost of prescription drugs, expand access to home energy upgrades, and tackle climate change. And importantly, it will create good-paying jobs right here in Vermont. Making sure this law–and the transformative programs within it–get implemented quickly and fairly will be key. No person, and no community, should be left out.” [Senator Peter Welch Press Release, 8/16/23]
Representative Steny Hoyer (D-MD-5): “A year later, America still feels the positive impacts of the Inflation Reduction Act. Inflation has fallen by two thirds since last summer. […] Additionally, thanks to the Inflation Reduction Act, 69.3 million seniors have saved money on their prescription drug costs, and the 16.3 million people who receive their health insurance through the Affordable Care Act are saving an average $800 a year on their health premiums. From capping monthly insulin costs for millions of Medicare beneficiaries to creating green jobs across the country, the Inflation Reduction Act is a cornerstone in Democrats’ Investing in America agenda.” [Representative Steny Hoyer Press Release, 8/16/23]
Representative Susan Wild (D-PA-07): “I’ve been taking on Big Pharma in the fight to get health care costs and drug prices down since my first day in Congress. The Inflation Reduction Act is a huge win in that fight. It’s making a real difference for Pennsylvania families and seniors by lowering health care costs, and by investing in clean energy and growing our economy. A year after I worked to pass the IRA into law, I’m keeping up the work to get costs down and build an economy that works for working people.” [Representative Susan Wild Press Release, 8/16/23]
Representative Jennifer McClellan (D-VA-04): “One year ago, President Biden signed House Democrats’ transformative Inflation Reduction Act into law. […] The IRA allowed Medicare to negotiate the price of certain prescription drugs for the first time, reduced the cost of insulin to $35 per month for seniors, and expanded affordable health care coverage to more Americans by enhancing subsidies under the Affordable Care Act and lowering premiums by an average of $800 per month. These are important steps in our continued efforts to ensure every American has access to quality, affordable health care and the life-saving prescription drugs they need. […] We have made tremendous progress since the IRA was signed into law, and we will continue to see the benefits of this legislation for years to come. As the provisions within the bill are implemented, I will work with the Biden-Harris Administration and relevant agencies to ensure Virginia’s Fourth continues to benefit from this historic legislation.” [Representative Jennifer McClellan Press Release, 8/16/23]
Democratic National Committee Chair Jaime Harrison, Democratic Senatorial Campaign Committee Chair Senator Gary Peters, and Democratic Congressional Campaign Committee Chair Representative Suzan DelBene: “Democrats took historic steps to address Americans’ most pressing priority: lowering costs on everything from prescription drugs to energy bills – all while helping grow jobs here in our country and tackling the climate crisis. While Democrats fought to lower costs, Republicans stood on the side of big drug companies, big oil companies, and other mega corporations that get rich by keeping prices high. Democrats remain committed to putting the interests of working families first. And that’s why voters will stand with Democrats in 2024.” [Democratic National Committee Press Release, 8/16/23]
EVENTS
President Joe Biden held a press conference delivering remarks on the anniversary of the Inflation Reduction Act. [White House Live, 8/16/23]
Majority Leader Chuck Schumer (D-NY) held a round table to highlight four different stories of how the Inflation Reduction Act is helping one year in. [X, 8/16/23]
Majority Leader Chuck Schumer (D-NY), Chair of the Finance Committee Ron Wyden (D-OR), and Senators Amy Klobuchar (D-MN), Debbie Stabenow (D-MI) held a press conference with AARP CEO Jo Ann Jenkins, Protect Our Care Executive Director Brad Woodhouse, and Irv Varkonyi, a Virginia senior on Medicare, celebrating the progress made to lower health care costs for Americans ahead of the one-year anniversary of the Inflation Reduction Act. [Facebook Live, 7/27/23]
HEADLINES
Newsweek: Opinion: Representative Pallone: Republicans Want You to Pay More for Medicine – Again. “One year ago this week, I joined President Joe Biden as he signed the Inflation Reduction Act into law. This transformational law finally reversed longstanding legal restrictions put in place by a Republican Congress 20 years ago that explicitly prevented Medicare from negotiating with pharmaceutical companies on the prices seniors pay for prescription drugs. Other nations negotiate lower prices for their citizens and so it’s only fair that the United States should be able to do the same. Negotiating drug prices is not only good for seniors’ wallets, making the lifesaving drugs they need more affordable, but also for taxpayers and national spending. The drug pricing reforms included in the Inflation Reduction Act are expected to cut the federal deficit by $237 billion over 10 years, saving taxpayers billions of dollars and extending Medicare’s solvency for years to come.” [Newsweek, 8/14/23]
New Hampshire Bulletin: Opinion: Expanding Affordable Health Care In New Hampshire. “One year ago, the Inflation Reduction Act became law. I’m thrilled to be traveling coast to coast on a national bus tour with Protect Our Care to celebrate that achievement, and to share the news about all the changes to our health care system in the past few years under the Biden administration. […] Under the Inflation Reduction Act, people on Medicare already have their insulin copays capped at $35 per month. The pressure from this measure has already forced insulin makers to lower the price of insulin for many people not covered by Medicare, too. […] The Inflation Reduction Act is only one of many ways in which the Biden administration is moving America forward on health care.” [New Hampshire Bulletin, 8/17/23]
ABC News: Biden Takes Victory Lap on Inflation Reduction Act Amid 2024 ‘Bidenomics’ Push. “At a celebration in the White House East Room, Biden branded the $740 billion climate, health and tax bill as one of the “most significant laws” ever enacted. “Taking on the special interests and winning,” the president said. “Delivering on promises that have long been made to the American people to lower cost for families, especially health care costs; increase America’s energy security; restore fairness to a tax code; create good paying jobs here in America; and to address the potential threat of climate crisis.” [ABC News, 8/16/23]
CNN: Biden Knocks GOP for Opposing His Domestic Agenda as He Celebrates Anniversary of the Inflation Reduction Act. “President Joe Biden celebrated the first anniversary of his administration’s signature climate and health care law on Wednesday – and knocked Republicans for opposing the measure during a lively event in the White House’s East Room. […] In his Wednesday remarks, Biden trumpeted provisions in the law that he pledged would cut carbon pollution in half by 2030, invest more than $50 billion to build up climate resilience and save Americans an average of $800 a year in health care premiums under the Affordable Care Act.” [CNN, 8/16/23]
Michigan Advance: Michigan Dem Leaders Tout Climate, Health Initiatives In The Inflation Reduction Act’s First Year. “The Inflation Reduction Act (IRA) of 2022, which set out to support the economy by curbing prescription drugs costs and investing in clean energy and electric vehicles, turned one year old Wednesday and Democratic leaders in Michigan joined together over Zoom to give a year-in-review. […] Gilchrist noted the IRA put a $35 cap on the monthly cost of insulin for Medicare beneficiaries, saying he’s witnessed people in his own family struggle to afford the insulin they need. […] More and more Michiganders will reap the benefits of health care reducing costs outlined in the IRA, Dingell said, with an estimated 673,000 Michiganders to save an average of $360 on prescription drugs annually starting in 2025 when more caps and drug reducing policies go into effect under the IRA.” [Michigan Advance, 8/16/23]
NY1 Spectrum News: ‘We’re Investing In All Of America: Biden Marks Anniversary Of Signing Landmark Climate, Health Care And Tax Law. “President Joe Biden marked the anniversary of one of his signature pieces of legislation on Wednesday – the so-called Inflation Reduction Act – calling it ‘one of the biggest drivers of jobs and economic growth this country has ever seen.’ […] Among the bill’s provisions are a $35 per month cap on insulin for Medicare recipients, reforms to allow Medicare to negotiate drug prices for certain medications, increased tax enforcement and a 15% corporate minimum tax rate, as well as the largest-ever federal investment to fight climate change. It passed both the Democratic-controlled House and Senate last year without any Republican support.” [NY1 Spectrum News, 8/16/23]
SOCIAL MEDIA
President Joe Biden: “Under the Inflation Reduction Act, folks on Medicare—no matter how many prescriptions they have—pay no more than $2,000 a year for their medication. This is a game-changer for American families.” [X, 8/16/23]
Senate Majority Leader Chuck Schumer (D-NY): “Since the Inflation Reduction Act became law: We made it possible for the first time ever for Medicare to negotiate the price of prescription drugs to bring down costs for seniors.” [X, 8/16/23]
Senate Majority Whip Richard Durbin (D-IL): “One year ago today, @POTUS signed the Inflation Reduction Act into law. @SenateDems fought tooth and nail for this historic legislation and for everyday Americans—to reduce costs for families, make the tax code fairer, and make the biggest climate action investment in history.” [X, 8/16/23]
House Democratic Leader Hakeem Jeffries (D-NY-8): “Insulin used to cost thousands of dollars per year for many older Americans. Dems passed the Inflation Reduction Act. Now it’s $35 per month.” [X, 8/16/23]
House Democratic Caucus Chair Pete Aguilar (D-CA-33): “One year ago, @HouseDemocrats passed the Inflation Reduction Act to lower health care costs for families, which included:
💊 Lower prescription drug costs
⚕ Lower health care costs
💉 $35/month cap on insulin” [X, 8/16/23]
Assistant House Democratic Leader James E. Clyburn (D-SC-6): “Today marks one year since @POTUS signed the Inflation Reduction Act into law — historic legislation to lower kitchen table costs, reduce prescription drug prices, shrink the deficit, and tackle climate change. That’s Bidenomics at work.” [X, 8/16/23]
Representative Jerry Nadler (D-NY-12), Ranking Member of the House Judiciary Committee: “One year ago today, @HouseDemocrats secured access to affordable health care for almost 15 million Americans. With the #InflationReductionAct, #NY12 residents are saving an average of $2,990 every year on their health insurance.” [X, 8/16/23]
Representative Nydia Velazquez (D-NY-7), Ranking Member of the Committee on Small Business: “One year ago, Democrats delivered the largest investment in clean energy in history. We empowered Medicare to negotiate drug prices and we secured lower health care costs. And we did it by making rich corporations finally start to pay their fair share. #InflationReductionAct” [X, 8/16/23]
Senator Jon Tester (D-MT): “A year ago today, we passed the Inflation Reduction Act to:
📉 Pay down the debt
💊 Slash prescription drug prices
🩺 Cap health care costs
🇺🇸 Invest in American energy
🌎 And protect our climate
ALL without raising taxes on Montanans, but by holding corporations accountable.” [X, 8/16/23]
Senator Mark Warner (D-VA): “One year ago, the Inflation Reduction Act was signed into law! It focused on the issues that matter: cutting health care costs for seniors, protecting miners’ benefits, lowering emissions, and slashing the deficit. Proud to have gotten it done for Virginians.” [X, 8/16/23]
Senator Tammy Duckworth (D-IL): “One year after @POTUS and Congressional Democrats enacted the Inflation Reduction Act, all have benefited from:
—Lower Rx costs
—$35/month cap on Medicare insulin costs
—Boosts in manufacturing and clean energy
—A fairer tax code
—Investments in climate action
—JOBS, JOBS, JOBS” [X, 8/16/23]
Representative Judy Chu (D-CA-28): “The #InflationReductionAct has also:
🩺Lowered health care costs
💊Capped prescription costs for Medicare beneficiaries
💡Driven down energy costs
@HouseDemocrats and I will keep fighting to continue this progress.” [X, 8/16/23]
Representative Ted Lieu (D-CA-36): “Since the #InflationReductionAct was passed one year ago, it has:
✔️Lowered prescription drug costs
✔️Created jobs and boosted the economy
✔️Lowered energy costs for families
Learn more about how this law is impacting our community: https://democrats-budget.house.gov/legislation/InflationReductionAct” [X, 8/16/23]
Representative Susie Lee (D-NV-03): “One year ago today, I voted for the #InflationReductionAct to give working folks the tools & opportunities to succeed.
In NV & beyond, those investments are:
🏥 Driving down health care costs
☀️ Creating 1000s of clean energy jobs
🌄 Protecting our public lands & water supplies” [X, 8/16/23]
Representative Lucy McBath (D-GA-07): “💊 Lower prescription drug costs
🏥 Lower health care costs
⚡ Lower energy costs
One year ago, my colleagues and I delivered the #InflationReductionAct to lower costs for American families—including a $35 insulin cap that I championed. We’re working to continue that progress.” [X, 8/16/23]





 Watch the event
Watch the event  Coverage:
Coverage: Coverage:
Coverage: Watch the event
Watch the event  Watch the event
Watch the event  Coverage:
Coverage: Watch the event
Watch the event  Watch the event
Watch the event