BREAKING: Biden-Harris Administration Announces Grantees Of $500 Million Investment Into ACA Navigators

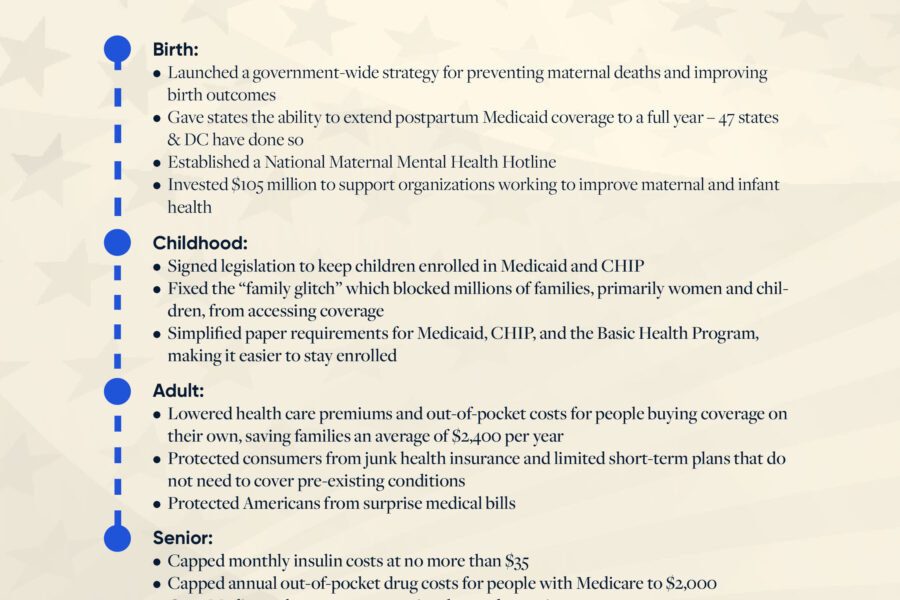
Historic Boost in Funding Will Help Secure Affordable Coverage for Millions of Americans Washington, D.C.…
ashoupAugust 26, 2024