U.S. Senators Bob Casey (D-PA), Tammy Baldwin (D-WI), and Peter Welch (D-VT), HHS Secretary Xavier Becerra, HHS Regional Directors Headlined Events Across Six States
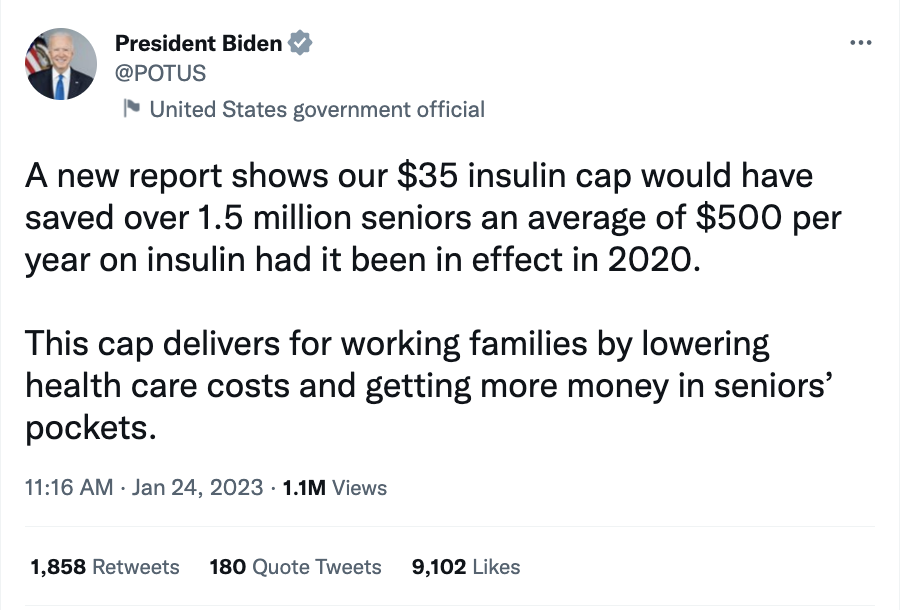
Over the last several weeks, lawmakers, administration officials, health care experts, and advocates joined Protect Our Care to discuss the new health care savings for the American people thanks to the Inflation Reduction Act. On January 1, critical provisions took effect, including extending lower health insurance premiums for those who bought through the ACA, capping the monthly cost of insulin at $35 for seniors, and providing needed vaccines, like the shingles vaccine, at no cost for Medicare beneficiaries.
During the events, speakers also discussed how the Inflation Reduction Act’s enhanced premium tax credits helped fuel a record-breaking open enrollment period, with 16.3 million people signing up for health care coverage on the ACA marketplaces. More than three million people are brand new to the marketplace.
Lawmakers have long promised to rein in high drug prices, lower health costs, and expand access — President Biden and Democrats are getting the job done.
ARIZONA
Wednesday, January 25 – Regional HHS Director and Will Humble Highlight New ACA Open Enrollment Numbers in Arizona: Dr. Jeffrey Reynoso and Will Humble joined Protect Our Care Arizona to discuss the record number of people who purchased ACA marketplace coverage with lower premiums for 2023 thanks to the Advanced Premium Tax Credits extended under the Inflation Reduction Act. This morning, the Department of Health and Human Services announced that 16.3 million Americans, including 235,229 Arizonans signed up for health insurance through the Affordable Care Act (ACA) marketplaces, including 3.1 million new enrollees. This represents a more than 12 percent increase nationally from the same time last year. “In Arizona the average middle class family of four is set to save $4,763 on their yearly premiums because of the IRA,” said Dr. Reynoso. “Arizonans heard the news and enrolled in record numbers. This is a trend that we saw nationwide.” Learn more about how the Inflation Reduction Act lowers health care costs for Arizonans here. A recording of the event can be viewed here.

Coverage:
- Cronkite News: Record numbers sign up for Obamacare health coverage in Arizona, U.S.
- White Mountain Independent: Record numbers sign up for Obamacare health coverage in Arizona, U.S.
- Arizona Public Media/PBS/NPR: Record breaking Affordable Care Act health insurance sign ups
GEORGIA
Friday, January 13 – Open Enrollment Event with HHS Regional Director Antrell Tyson, Georgians for A Healthy Future, and Health Care Advocates: Experts from Georgians for a Healthy Future and the U.S. Department of Health & Human Services joined Protect Our Care Georgia to discuss the ACA Open Enrollment 2023 period – which started on November 1, 2022 and ends on January 15th. “Just like the Bulldogs’ victory on Monday night, this year’s open enrollment has already proven to be a huge victory for thousands of Georgians,” said Health and Human Services Regional Director Antrell Tyson. “Georgia residents without health insurance through their jobs have the opportunity from now, until Jan. 15, to enroll in comprehensive health coverage. The time is now,” he added. You can watch the event here.

Coverage:
- Capitol Beat: Georgia Affordable Care Act enrollment soars
- WALB (NBC/ABC): Affordable Care Act open enrollment deadline approaching
- Insurance News Net: Georgia Affordable Care Act enrollment soars
- The Douglas Sentinel: Georgia Affordable Care Act enrollment soars
- The Christian Index: Georgia Affordable Care Act enrollment soars
- The Augusta Press: Georgia Affordable Care Act enrollment soars
- The Morgan County Citizen: Georgia Affordable Care Act enrollment soars
- The Albany Herald: Georgia Affordable Care Act enrollment soars
- Business Insurance: Georgia reports record enrollment in ACA marketplace
- The Marietta Daily Journal: Georgia Affordable Care Act enrollment soars
- The Walker County Messenger: Georgia Affordable Care Act enrollment soars
- The Catoosa County News: Georgia Affordable Care Act enrollment soars
- The Rome News Tribune: Georgia Affordable Care Act enrollment soars
- The Calhoun Times: Georgia Affordable Care Act enrollment soars
- Polk Standard Journal: Georgia Affordable Care Act enrollment soars
- The Gwinnett Daily Post: Georgia Affordable Care Act enrollment soars
- WFXL: Georgia Affordable Care Act enrollment soars
- The Jackson Press Argus: Georgia Affordable Care Act enrollment soars
- The Henry Herald: Georgia Affordable Care Act enrollment soars
- The Rockdale Citizen: Georgia Affordable Care Act enrollment soars
- WALB (NBC/ABC): Affordable Care Act open enrollment deadline approaching
MICHIGAN
Thursday, January 26 — Health Care Leaders Celebrate Successful Michigan Open Enrollment Numbers and Costs Savings in 2023: Health care leaders joined Protect Our Care Michigan to celebrate a record-breaking enrollment of 322,273 Michiganders into the ACA marketplace for 2023. This year seniors in the state and across the country are saving on insulin costs and life-saving vaccines thanks to the Inflation Reduction Act. “The Inflation Reduction Act has been nothing short of a game changer in our community,” said Jim Ananich, President and CEO of the Greater Flint Health Coalition. “The monthly cap on insulin for Medicare recipients is a lifesaving benefit in communities of color like Flint disproportionately impacted by diabetes. Along with providing our seniors with shingles and other critical vaccinations at no cost, this landmark law is taking a major step toward reducing racial inequities in health care in our community and beyond.” You can watch the event here, and learn more about how the Inflation Reduction Act is keeping costs low for Michiganders here.
Coverage:
- Detroit Free Press: Michigan sees highest Obamacare enrollment since 2016
- MLive: Record Michiganders seek health insurance through ACA marketplace in 2023
- WXMI-TV, Fox – Grand Rapids: Newsclip
- Gongwer: Health Care Leaders Boast Record-Breaking Open Enrollment
NEVADA
Tuesday, January 24 — U.S. DHHS Regional Director, Nevada Health Link Director Highlight ACA Open Enrollment Numbers in Nevada: Dr. Jeffrey Reynoso, U.S. Department of Health and Human Services Regional Director, and Ryan High, Executive Director of Nevada Health Link, joined Protect Our Care Nevada to discuss the record number of people who purchased ACA marketplace coverage with lower premiums for 2023 thanks to the Advanced Premium Tax Credits extended under the Inflation Reduction Act. “Americans know a good deal when they see one,” said Dr. Jeffrey Reynoso. “Thanks to the enhanced premium tax credits included in the Inflation Reduction Act, more people than ever signed up for health insurance during the 2022 open enrollment period. These tax credits will save an average middle-class family of four in Nevada $4,494 on their yearly premiums, giving them the breathing room to pay for other necessities like food, gas, and rent.” Learn more about how the Inflation Reduction Act lowers health care costs for Nevadans here. A recording of the event can be viewed here.

Coverage:
- KRXI (Reno Fox): Nearly 100,000 Nevadans signed up for health insurance this year
- KRXI (Reno FOX): Record-Breaking Open Enrollment Numbers
- KTVN (Reno CBS): Record Open Enrollment for Nevadans
- KTVN (Reno CBS): Open Enrollment in Nevada
- KRNV (Reno NBC): Record-Breaking Open Enrollment Numbers in Nevada
- KTNV (Las Vegas ABC): ACA Enrollment
- Nevada Current: Opinion: Affordable health insurance empowers us all
PENNSYLVANIA
Wednesday, January 25 — Senator Bob Casey, HHS Region 3 Director Dr. Ala Stanford, and Health Care Advocates Highlight How the Inflation Reduction Act Caps Insulin Costs and Expands Access to Free Vaccines for Seniors: Senator Bob Casey, Dr. Ala Stanford, and health care advocates joined Protect Our Care Pennsylvania to highlight how seniors in Pennsylvania and across the country are saving on insulin costs and life-saving vaccines thanks to the Inflation Reduction Act. “Because of the Inflation Reduction Act, an estimated 261,000 Pennsylvania seniors can now access life-saving vaccines at no cost and 87,000 Pennsylvanians are starting to see reduced costs for their insulin. These are huge milestones, and I’m proud to have fought for these provisions alongside Protect Our Care, which has been an incredible partner in protecting health care across the Nation,” said Senator Bob Casey (D-PA). “Families shouldn’t have to choose between their health and their bank account. We still have more work to do, and I will continue to fight in Washington to help Pennsylvania families and seniors save on health care costs.” You can watch the event here, and learn more about how the Inflation Reduction Act is keeping costs low for Pennsylvanians here.

Coverage:
- WOLF (Hazleton FOX): Senator Casey Highlights Inflation Reduction Act Savings
- WOLF (Hazleton FOX): Senator Casey highlights savings from the Reduction Inflation Act
- WCAU (Philadelphia NBC): Medicare Patients to See Savings on Insulin & Vaccines
- WPVI (Philadelphia ABC): Inflation Reduction Act Benefits
- KYW Newsradio: Inflation Reduction Act Savings on Insulin & Vaccines
- KYW Newsradio: Medicare beneficiaries across Pa. can expect to see big savings on insulin and vaccines
VERMONT
Monday, January 9 — HHS Secretary Becerra, Senator Welch, and Health Care Advocates Celebrate Inflation Reduction Act Provisions to Drive Down Drug Prices: U.S. Senator Peter Welch (D-VT) and Health and Human Services Secretary Xavier Becerra joined health care advocates in Rutland, Vermont, for a press conference celebrating prescription drug pricing provisions in the Inflation Reduction Act. “Already today, there are probably Vermonters who have bought insulin for $35 thanks to the Inflation Reduction Act,” said HHS Secretary Xavier Becerra. “The president said one thing on health care when he was campaigning and he said it again at his inauguration: we’re going to lower costs for more Americans with better benefits — and that’s exactly what he has done.”
 Coverage:
Coverage:
- WCAX: Top Biden official joins Welch in Rutland to talk prescription drug and opioids
- NBC5: Sen. Peter Welch’s 1st day on the job: The Inflation Reduction Act
- Rutland Herald: Welch: Medications are about to get cheaper for many on fixed incomes
WISCONSIN
Thursday, January 12 — Shingles Vaccine and Insulin Affordability Roundtable with Senator Tammy Baldwin and Wisconsin Seniors: Senator Tammy Baldwin joined Protect Our Care Wisconsin alongside Seniors from Green Bay and Appleton to highlight how Medicare enrollees are already benefiting from the Inflation Reduction Act, which took effect this month and is lowering costs improving health care for millions of Americans. “Too many Americans are seeing the costs of their prescription drugs increase and are struggling to afford the medications they need to survive,” says Senator Baldwin. “That’s why I was proud to support the Inflation Reduction Act last year, to finally provide some relief for Wisconsin families and hold drug companies accountable for prioritizing profits over people.” You can watch the event here.

Coverage:
- Press Times: Local seniors discuss impact of new healthcare provisions